Gaining insights into the potentially long-term and long-lasting effects of COVID-19 that sees up to 57% of sufferers struggling with symptoms for up to six months, or longer, for reasons the medical establishment doesn’t yet understand.
Whether you've personally had COVID-19 or not (I have), or if you know someone who has, chances are you probably know someone who has suffered some longer-lasting physiological challenge or symptom since getting sick.
For one of my best friends, it’s the sense of smell, or more precisely, it’s the fact that he still has a difficult time when it comes to smelling things some six months on.
For others, it turns out it can be any one of a number of ongoing, chronic symptoms, that not only last for weeks after the actual illness stops, but in some cases, can last for months.
Although I was somewhat aware, osmosis-wise, that such a thing could occur, I had never come across an actual term or description of these lingering COVID symptoms until a week ago Wednesday. And on that day, I happened upon not one, but two references to this phenomenon, something called Long COVID.
And in one instance, it was found in a news release from Orem, Utah-based NOMI Health announcing the launch of its Long COVID Care Management Program.

So it was that I found myself visiting yesterday afternoon for about a half-an-hour with one of NOMI Health’s Medical Directors (June Steely, MD) to talk about this medical mystery that I now realize has many names, but simply put, is a form of chronic, long-term symptoms of COVID-19.
But rather than try and crystalize our conversation into a typical long-form article, I thought it might be more informative to instead share the bulk of that conversation here in a Q&A format.
So, with minor edits for clarity’s sake and to improve readability, here is that conversation.
A Silicon Slopes Conversation Between David Politis and NOMI Health’s Dr. June Steely About Long COVID
David Politis (DP): David Politis here with Silicon Slopes Conversations. With me today is Dr. June Steely, medical director with NOMI Health. That means you're the big kahuna.
June Steely, MD (JS): I don't know that I'd say that. I certainly have other people who collaborate with me who are other medical directors.

DP: Well, welcome. We're here today to talk about a specific thing that I recently learned about called Long COVID.
Obviously, coronavirus has been in the news for over two years. As we were talking earlier, I got COVID way back in January 2020 after going to this major trade show with 165,000 of my closest friends, and I was sick as a dog for 10 days. Coronavirus is not a fun thing, right?
JS: Absolutely not. You do not want to have it if you can avoid it.
DP: I recently read this story in Wired magazine, of all places, about Long COVID. And then later that same day, I saw this announcement from NOMI Health that talked about what NOMI is doing to help its clients, both large corporations and government organizations, to help them with monitoring Long COVID. And I thought, okay, I need to reach out to this company.
So officially, it's known as Post-Acute Sequelae of SARS CoV-2 Infection. What the heck does that even mean?
JS: It's a lot easier to say “Long-Haulers,” people who have had symptoms for the “long haul.” Or Long COVID is another way it's most commonly referred to.
DP: What does it mean to be a “Long-Hauler,” to have Long COVID or Post-COVID? What does that even mean?
JS: The majority of people luckily get sick, have somewhat mild—although you yourself know that they're not that mild—symptoms, and recover within a couple of weeks. Some people get very sick. Have to be in the ICU, stay there for weeks to months and then have a very long recovery and continue to have symptoms. Now, those people are one type of people that we would consider Long COVID sufferers.
But there's another kind of people. And these are usually younger patients who get sick or maybe they're not even sure they had it. But then weeks to months later continue to have symptoms that are debilitating. And those folks are luckily not as common as people having continued symptoms for a long time after they've been in the hospital.
But they're there and they have gone from being completely functional—they're usually young, in the prime of their lives—to having very debilitating symptoms daily.
DP: When I think about COVID, coronavirus, COVID-19 (tying back, of course, to the year that it first emerged over in China—in spite of some protestations out of the People's Republic), I think of mostly respiratory sickness. And I think the challenges for those that tend to be older—45, 55, and above.
And then where it gets really tricky is with those who have what are known as comorbidities. Now, real simply for our audience out there: What is a comorbidity?
JS: Comorbidity is a chronic condition that you have that makes you more likely to have severe disease. So hypertension or high blood pressure; having had a heart attack in the past; having diabetes. Those are each comorbidities.
DP: So you have somebody who has a chronic disease or a chronic condition. COPD, of course, would be one. Someone who's had pneumonia, walking pneumonia, not a good thing, right? Emphysema would not be a good thing, right?
Obviously those would be bad. So these are individuals typically that are middle-age or above. But you said moments ago that when it comes to Long-Haulers, that in fact it can be those who are in the prime of life or even younger. What's going on here?
JS: Well, we wish we understood that. You know, there is speculation that the virus triggers the immune system to produce inflammation in the body for months afterwards. We are studying that, of course, everybody wants to know. So we're studying it. We don't understand it, but we've noticed it. And we're trying to help those people.
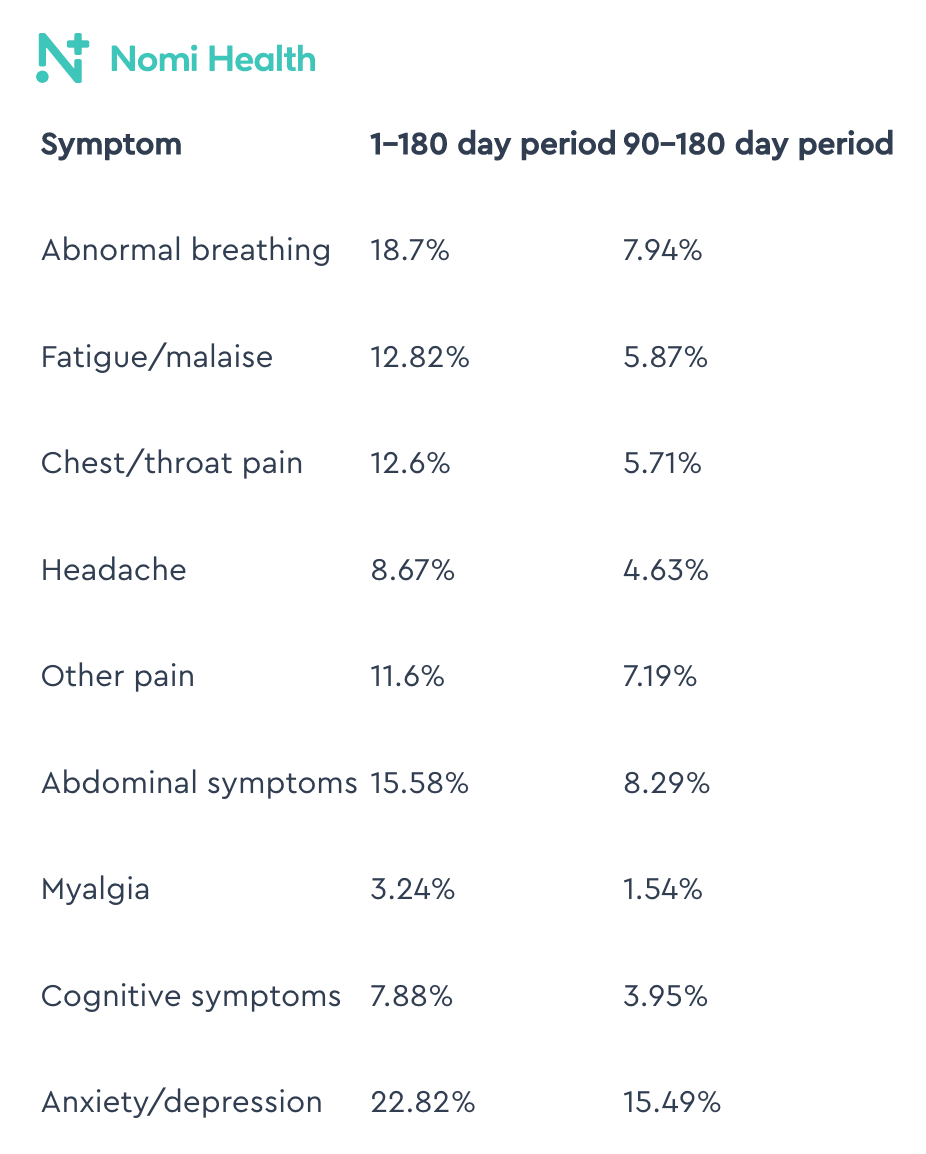
DP: And for these individuals, with what I'm seeing (and in fact, part of what’s included on the NOMI Health website), shows what happens symptomatically. And you give examples of what happens between 1–180 days after disease onset and what happens at 90–180 days. So basically the first quarter to the second quarter after someone has COVID.
And there's some stuff on here that makes sense: abnormal breathing, chest and throat pain. Okay. But then it gets into stuff like
- Abdominal symptoms, and
- Cognitive symptoms, and
- Anxiety and depression.
And in fact it says that for those that upwards of 22% of people who are Long-Haulers suffer from some form of anxiety or depression. Can you talk about that?
JS: Yes, I think that's, you know, a result of the illness. They are used to being productive individuals who can do what they want to do, exercise when they want to exercise. They can, you know, go to work, get stuff done. And now they find their ability to do those things is limited. And of course that would make anybody feel down and depressed.
DP: Okay, okay. It's not necessarily that it's attacking your central cortex or anything? Or maybe?
JS: There has been some of that, too. There have been studies that show that COVID has affected the brain, including the place in our brain where we sense smell. So, yes, there are some. It can be part of the disease, but it can also be in reaction to the disability.
DP: With one of my best friends, COVID hit their family probably seven months ago. It ran through all the kids, the parents, and my friend still says to this day, “I can't smell everything, or it doesn't smell right.” So obviously smell is tied to the central nervous system.
JS: Yes. And there have been some scans showing that there is damage to that area of the brain that can persist for a long time.
DP: So how then is the long-term symptom showing up for some individuals with abdominal pain? I don't understand that.
JS: That could be nausea, some vomiting, or just discomfort. The virus can, you know, affect the intestinal function also. And again, we don't understand it all. It's a pretty new disease.
DP: So what about those who are younger?
And let me break those into two categories:
- Pre-20 (the teenagers) and then
- Those who are younger.
What should parents be concerned about with regards to Long-Term COVID, Chronic COVID for their children?
JS: Well, luckily, it is less common the younger you get. And they are likely to recover more quickly, the younger they are also. But you know, certainly watching their level of activity:
- Are they still able to run around on the playground like they used to?
- Are they still able to participate in sports?
- Do they seem to be having a harder time at school because they're having trouble concentrating?
Those would be symptoms to look for.
DP: So they're literally saying that for some kids who have had COVID, school is harder for them because they can't concentrate. They can't stay on point. Is that right?
JS: That's correct. Luckily, it is not as common in children, but it has been observed.
DP: Are they seeing a similar challenge for adults with lack of ability to focus or lack of energy?
JS: The term is “brain fog.” It’s how people like to describe it.
DP: Has this been added to the lexicon for medical professionals?
JS: Well, I don't think it was come up with by a medical professional, but it is certainly something that we hear and that people say and can kind of understand.
DP: I feel that way when it gets really warm in the spring, and I get a “brain fog” about work. You're not talking about that, right?
JS: I'm talking about tasks that used to be easy for you to do, cognitively. Things at work or well, people don't balance their checkbook anymore, but you know, that type of thing, that they find it more difficult since having COVID.
DP: But can it be also memory, just straight up memory? Like, it’s harder to recall a given name. Harder to recall that phrase or whatever.
JS: Yes, it can be that, too.
DP: So in simple terms, what NOMI has done is they've said, “We're seeing this. We're involved in trying to help change the role of insurance in health care and providing greater ability for individuals and for employers to lower health care costs and to help individuals take more control of their health care.” That's a general level description of what NOMI is about, correct?
JS: That's correct. And Long COVID has really interfered with the lives and livelihoods of millions of Americans.
DP: Do we have a sense of how many Americans may actually be struggling with some form of Long COVID today?
JS: I've certainly seen numbers, but it's really difficult to tell. And luckily, most people do get better. And so the numbers would change from week to week.
DP: So it's more than two and less than 330 million.
JS: I’ve seen (figures of) between three [million] and 23 million Americans.
DP: Seriously?
JS: Yes. Between three [million] and 23 million Americans are the numbers I've seen.
DP: Wow! Okay. So on the one end, it's 1%. So it's bad, but it's not really bad. But if it's 23 million, you're upward of 6% to 7% of the population. Really?
JS: Well, like I said, I don't know.
DP: This is not a U.S. thing, though?
JS: No, it's not only in the U.S.
DP: So, you're seeing this around the world, regardless of economic strata, regardless of race, regardless of culture, and to some extent, regardless of age, correct?
JS: Yes.
DP: So then what's an adult supposed to do? What's a parent supposed to do? What's a caregiver supposed to do if they themselves notice that, “You know, gee, it's been a week-and-a-half, two weeks, three weeks, three months. I'm struggling with abnormal breathing, fatigue, malaise, chest, throat, pain, headache, other pain, abdominal symptoms, myalgia, cognitive symptoms, or anxiety and depression.” What are they supposed to do?
JS: Well, I would recommend that they see a health care provider and have them help determine “Is this Long-Term COVID? Or is this something else?”
DP: Is there a test that can actually tell you if you have Long-Term COVID?
JS: No. It's a diagnosis of exclusion with the right symptoms in the right circumstance. So unfortunately, no, there's not a blood test that says you have it or you don't have it.
DP: And diagnosis of exclusion is: you are looking to show you don't have pneumonia. You don't have whooping cough. You don't have whatever else.
JS: Some things that could mimic, say, anemia. And so they would want to do a blood count to make sure you have enough blood cells. Or low thyroid levels, so they might want to do that type of test, too.
DP: We're not going to get rid of COVID, are we?
JS: Unfortunately, no.
DP: Coronavirus is here to stay and has been for a couple of decades, right?
JS: Well, yes, not COVID-19, but yes. SARS and different Coronaviruses. Yes.
DP: So it then becomes just part of the fabric of our life.
JS: Unfortunately.
DP: So in closing then, I'm assuming that you’re going to say, “If you're not vaccinated, go get vaccinated.”
JS: That's true. And even if you have Long COVID, if you get vaccinated, it will not make your symptoms worse. In some studies, it made them better.
DP: But obviously, basic stuff. Wash your hands regularly, religiously, some would say, correct?
JS: Correct.
DP: Avoid being in large crowds, if you can, right?
JS: Correct.
DP: And are you a believer in masks and masking?
JS: I am, especially if you're going to be in close quarters with a lot of people and there's a high prevalence in the community, a high prevalence of people of COVID.
DP: And what other things would you tell someone, last-minute, as far as we've had this conversation today? What else can you do to try to help yourself with regards to just coronavirus and being healthy, period?
JS: As far as coronavirus goes, all the things you said: get vaccinated, avoid it. As far as if you think you have Long COVID, then I think a support system that can really help you, that can say, “I believe you. This isn't all in your head. You're not alone. I can't cure you. But here are some things I can do to help you cope.”
DP: Okay, fair enough. Dr. June Steely of NOMI Health, I appreciate you coming in today and talking to us about Chronic Coronavirus, Chronic COVID, Long-Term COVID, Post-COVID syndrome. I mean, on and on and on.
This is David Politis with Silicon Slopes Conversations. Thank you for joining us today.
AUTHOR’S NOTE: I also found this article from the American Medical Association about Long COVID to be very informative. It’s titled “What doctors wish patients knew about long COVID”.