Newly cleared by the FDA, the Novarad augmented reality system revolutionizes the ability of spinal surgeons to deliver pinpoint surgical accuracy and hails the not-too-distant day where each medical incision may be assisted using AR solutions.
I have to be honest: At times, the scale and pace of technological, medical, and scientific advancement makes it hard to not become jaded, even inured to all of the change I have seen and lived through as a journalist, marketer, and communications professional during the last three-and-a-half decades.
And yet, every once in a while something will pop-up on my radar that makes me pause and wonder, “What in the world is that?”
That happened recently when I read a news release headline announcing that the U.S. Food and Drug Administration had given marketing clearance to the augmented reality system developed by a Provo, Utah-based firm that can now be used in spinal surgeries.
The headline did what it was supposed to do: It stopped me in my tracks and led me to read further, which I did, which in turn led me to a whole bunch of questions.
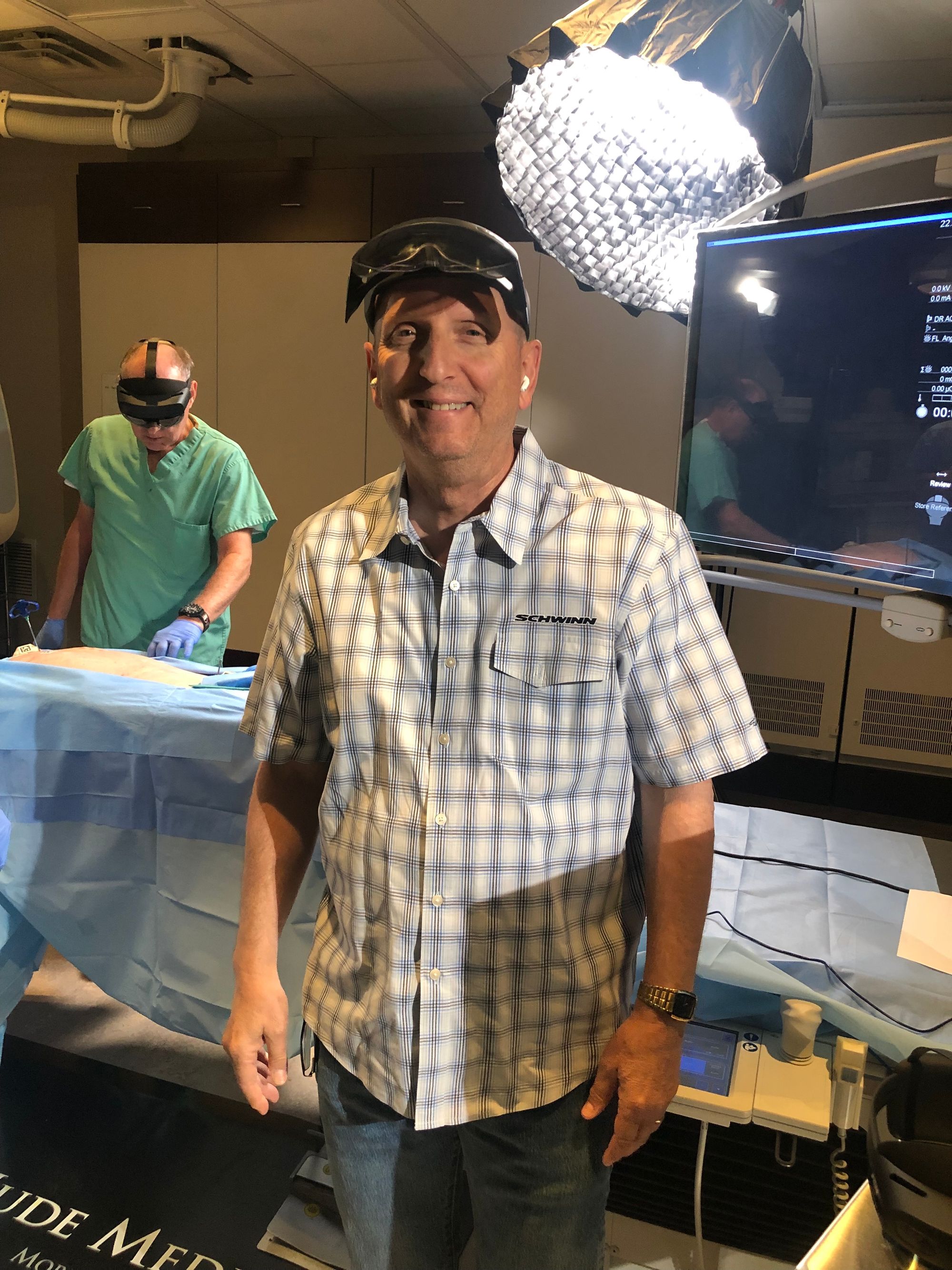
But more importantly, I found myself a few weeks back in a surgical suite in the Provo headquarters of a company called Novarad testing out its VisAR system for myself, with the AR headset tightened onto my head, visor down, as I called out commands and pinched fingers in midair to maneuver in-body images showing exact positions of the spine, rib cage, and tagged needles penetrating the cadaver.
It. Was. Mind-blowing!
More importantly: It. Is. Healthcare-changing.
No question about it.
Here then is the story of Novarad.
From Childhood Tinkerer to Radiologist and from Inventor to Entrepreneur
Wendell Gibby was born in Idaho, but raised in Orem, Utah, and based upon my recent conversation with him, he sounds like the classic super smart, yet somewhat precocious, tinkerer.

In fact, while in junior high school back in the 1970s, he and his “nerdy friends” were building boxes that transformed modulated sound into various colors of light to produce strobe-light shows when rock and roll music was played.
Gibby received his bachelor’s degree in chemistry from Brigham Young University before receiving his doctorate in medicine from the University of Utah. Post-doctoral training included an internship in internal medicine at UCLA, a residency at the University of Arizona, and a neuroradiology fellowship at the University of Pennsylvania.
After finishing med school, Dr. Gibby started synthesizing magneto pharmaceuticals for use at work, and later he launched a laboratory in an empty space he found at UofA as he started creating polymeric chelates for MRI imaging.
Although he has had several different business ventures throughout his career, including launching Blue Rock Medical in northern Provo, Dr. Gibby launched Novarad in 1988, the year after completing his radiologist training at the University of Pennsylvania.
Initially, Novarad was a teleradiology company, meaning it allowed the viewing of radiology imagery outside of a healthcare setting via the internet / world wide web.
From my perspective, however, the Novarad story begins to become compelling six years ago in 2016, for that’s the year Microsoft shipped its first iteration of HoloLens.
Augmented Reality: From Concept to Mass Market Reality
In spite of some confusion in the marketplace, virtual reality and augmented reality are not the same thing.
In the case of VR, visual imagery is produced in a closed, immersive environment (generally accompanied with sound, and sometimes with some type of tactile feedback), while simultaneously blocking out external stimuli to trick the human mind into believing that a virtual world is actually real.
Perhaps today’s most widely known example of a VR solution is Meta’s Oculus gaming system.
Conversely, with AR systems the intent is not to block out the external world, but rather to add to it with imagery and sound, and perhaps with other sensations as well. In other words to augment the real world.

In the case of Novarad, when Microsoft announced in mid-2015 that it was coming out with its own VR/AR platform, Novarad CTO, Steven Cvetko, Ph.D. paid special attention as he foresaw the potential for the HoloLens to solve an imaging problem for radiologists and surgeons.
Specifically, for as long as medical imaging technology has existed, it has had two primary drawbacks:
- The complexity of producing (and the time, systems, and the trained professionals required to create), useful radiographic imagery, and
- The general difficulty of relating such images to the patient in an operating room setting.
To their respective credit, Dr. Cvetko was insistent on the prospect the HoloLens might hold for Novarad in projecting holographic imagery inside patients in surgical suites, while Dr. Gibby was willing to give him free rein in making that initial HoloLens purchase to see if he could transform radiological input into heads-up display functionality.
The short answer is that now, some six years on, Novarad has a growing list of surgeons and radiologists that are blown away by the visual acuity and surgery-enhancing capabilities the VisAR system delivers.
More importantly, Novarad has now received marketing clearance from the U.S. Food and Drug Administration for use of the VisAR system in spinal surgeries.
And as Dr. Gibby and Dr. Cvetko explained to me recently, the company is already significantly down the road in pursuing FDA clearance for use in other surgeries, notably in cranial and oncology settings, among others.
My Personal Experience with Novarad’s VisAR
On a Saturday morning roughly one month ago I visited Novarad’s facilities in Provo to experience the VisAR firsthand a few days before my in-studio interview with Dr. Gibby.
That particular morning, Novarad had two cadaver torsos on hand for first person demonstrations for a number of surgeons, one of which had traveled from Israel to experience the VisAR for himself in a mocked-up surgical suite.
In this regard, virtually all of my interaction with Novarad personnel on this particular day was with members of its business development and marketing teams, with some one-on-one time spent with Dr. Cvetko.
For all intents and purposes the VisAR hardware is virtually identical from a physical standpoint to the Microsoft HoloLens 2, with the exception of Novarad branding. The differences are clearly on the software side of the equation.
According to the Novarad website,
“VisAR transforms a patient’s imaging data into a 3-dimensional hologram which is visible through an optical visor and superimposed onto the patient with submillimeter accuracy.”
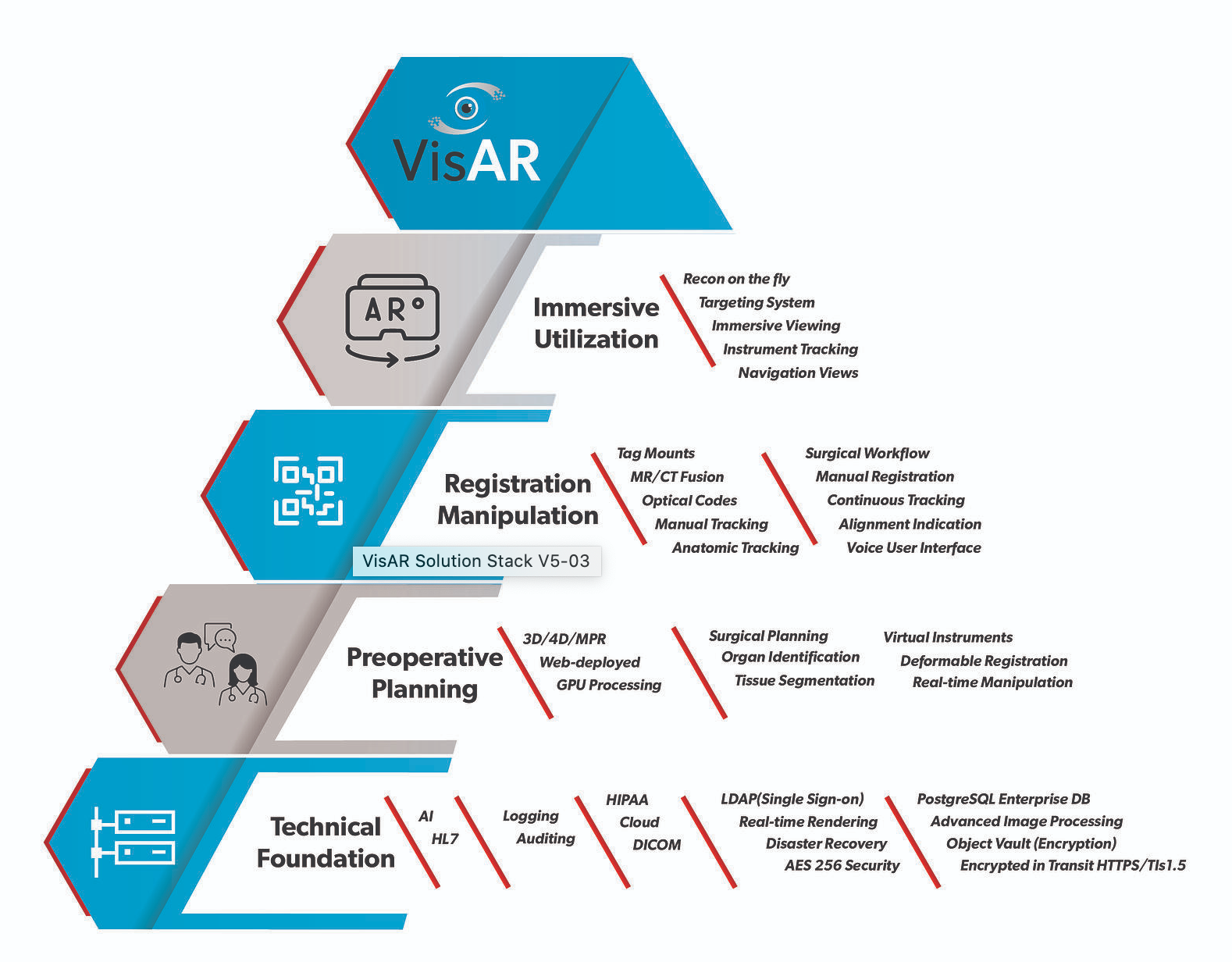
The VisAR system’s full technology stack includes:
- An object Store,
- Encryption at rest and in transit,
- HIPAA logging,
- LDAP login,
- Remote diagnostics and configuration,
- Advanced security,
- Advanced AI powered segmentation,
- Virtual tools, and
- Augmentation tags.
VisAR is also capable of multiuser settings, which allows for multiple operating room participants to see the same viewpoint simultaneously. It also enables enhanced student and resident training as well.
The expected launch time and set-up for the VisAR in an operating room is ~2 minutes, which was my experience at Novarad.
Once I adjusted the VisAR onto my head and lowered the visor in place in front of my eyes, I was able to instantly see a holographic representation of the spine and rib cage displayed in my field of view to create a cutaway- like imagery layered on the cadaver torso.
When I moved my head, the holographic representation moved as expected. And if I wanted to see a different perspective, I merely uttered the appropriate voice command to see
- A bone and tissue representation,
- A top-down orientation, or
- An orthogonal viewpoint looking directly down length of the spine.
I could also pinch my thumb and forefinger within my field of view to make the image shrink, while doing the opposite produced a tighter/closer viewpoint.
As needles had been inserted into the cadaver to simulate their placement during surgery to help guide the surgeon, I could clearly see their placement as well. In fact, Novarad says the VisAR’s navigation accuracy is less than two millimeters today.
Although clearly not a radiologist or surgeon, I found the VisAR quite simple to use and dramatically powerful in the rapid and simple way it provided detailed holographic imagery to enhance a potential surgical experience for me.
Officially, the FDA’s 510k notice for VisAR is for “stereotactic surgical guidance,” which, in plain English means that the imagery provided by the VisAR system is enhanced and guided by insertion of foreign objects into the body, aka, needles, which then produce guidance accuracy at less than two millimeters.
When asked about the prospect of gaining FDA clearance for other surgical applications, Dr. Gibby said,
“I think the promise of (VisAR), and we’re realizing this, is adaptability to lots and lots of organ systems. Cranial and spine are two typical ones that use guidance, (but others include) joints, plastic surgery, ENT.
“Once you cut into the body it’s just kind of a bloody field. You don’t really have this precise ability to see, especially if you’ve been in there before, it’s scar tissue. (So) you’re trying to find that lymph node, that tumor, that fracture.
“So surgeons have required larger exposure fields, more dissection, more tissue trauma, which means more risk, more recovery time. But if we can make that surgery smaller, more keyhole approaches, more targeted to the area of interest, it’s better patient care.”
“The challenge,” he added, “is we have great guidance technology today, but it’s slow. It takes 45 minutes to set-up in an OR. It takes a team of people. You have to drag all of this equipment into the room.”
Dr. Gibby also explained that these large, bulky, slower systems are also not easily transported and set-up in an Emergency Room or a field hospital or inside an ICU.
Additionally, he explained,
“If you’re at a small hospital in Nebraska, you (probably) can’t afford a $2 million robot. But they probably could afford a $3,500 headset.”
= = = = = = = = = = = = = = = = = = = = = = = = =
The Politis Perspective
If you haven’t guessed by now, I am a huge fan of Novarad and its VisAR augmented reality surgical enhancement solution.
Although the VisAR is only cleared for pre-surgical planning and in targeted spinal surgeries currently, the writing is clearly on the wall as far as I am concerned.
To me there are only two questions that matter today:
- How long will it take Novarad to apply for new surgical clearances? and
- How long will it take the FDA to clear new use cases?
From my perspective, Novarad is clearly a Utah MedTech company to watch.
AUTHOR'S NOTE: To watch my interview of Novarad's Dr. Wendell Gibby, please click here to watch this episode of “Conversations” on SiliconSlopes.tv. Conversely, you can also listen to this interview on your favorite podcast provider at “Silicon Slopes Conversations;” case in point, via this link on Apple podcasts or via most popular podcast platforms.
Thank you.








